BACKGROUND:
Acute myeloid leukemia (AML) is a highly heterogeneous group of diseases with variable response to therapy. Several factors have a prognostic impact for an outcome. Despite intensive chemotherapy and hematopoietic stem cell transplant (HCT), a significant proportion of patients eventually relapse, indicating that morphological assessment is not adequate due to limitations in sensitivity, requiring a better tool for assessment of remission.
METHODS:
A retrospective analysis was performed in AML patients who achieved first complete remission (CR1) and the outcomes compared according to the performance of HCT, and multi-color flow cytometry (MFC)-based measurable residual disease (MRD) status (defined as negative if patients achieved 0.1% or less) assessed at the time of CR1.
In order to take account of the time interval from the MFC-MRD assessment to HCT, we applied a Mantel-Byar test for overall (OS) and relapse-free survival (RFS), considering time-to-HCT as a time-dependent covariate, while Simon and Makuch plot was used. Time-dependent Cox proportional hazard models were applied for multivariate analysis. Cumulative incidence of relapse (CIR) and non-relapse mortality (NRM) where evaluated using Fine-Gray model.
RESULTS:
A total of 435 patients diagnosed with AML and treated with induction chemotherapy between 2015 and 2018, of whom 380 patients (87%) achieved remission, were included. MFC-MRD was assessed in 336 patients in CR1 (77%), out of 380 patients who achieved CR1, and 200 patients (53%) proceeded to HCT.
We evaluated OS, RFS, CIR and NRM according to MFC-MRD status in those patients who had negative MRD (MRDneg; n=218, 65%) vs. those with MRD (MRDpos; n=118, 35%). The OS at 2 years was 67.0% vs.40.7% (p≤0.001), RFS at 2 years was 8.7% vs. 40.6% (p≤0.001), CIR 26.9% vs.21.1% but with borderline significance (p=0.08), and NRM 32.5% vs. 20.2% with borderline significance (p=0.057).
In patients who achieved CR, we compared OS, CIR, NRM and RFS between the HCT group (n=200) vs. those who did not undergo HCT (no-HCT; n=235). Between the 2 groups, the OS at 2 years was 55.7% vs. 47.2% (p=0.004); CIR 9.7% vs. 34.6% (p≤0.001); NRM 40.9% vs. 12.6% (p≤0.001). There was no difference in RFS: 49.4% vs. 52.8% (p=0.505).
There was no difference in the time interval from the MFC-MRD assessment to HCT between the groups (MRDpos vs MRDneg) with a median of 96 days in overall patients who received HCT (p=0.31).
In the overall population, when HCT was accounted as a time-dependent covariate, we failed to observe any difference of OS (HR 1.23; p=0.19) or RFS (HR 1.09; p=0.60) between the HCT vs. no-HCT groups.
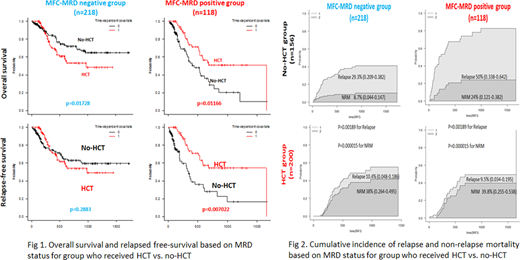
Then, we compared the OS, RFS, CIR, and NRM between the HCT vs no-HCT groups confined to the subgroups of patients with MFC-MRDneg vs MFC-MRDpos, separately. In the MFC-MRDpos subgroup, patients who underwent HCT did better: OS 54.8% in HCT vs. 25.5% in no-HCT (HR 0.52; p≤0.001) and RFS 48.7% vs. 24.1% (HR 0.45; p≤0.001). However, in the MFC-MRDneg subgroup, similar outcomes were noted between the HCT vs no-HCT groups in terms of OS 60.8% vs. 70.7% (HR 1.27, p=0.32), RFS 51.6% vs. 62.4% (HR 1.25; p=0.46) (Fig 1).
With respect to the cause of treatment failure according to treatment modality (HCT vs no-HCT) and MFC-MRD status, Fig 2 revealed different patterns of relapse vs NRM between the HCT and the no-HCT groups. In the MFC-MRDneg subgroup, HCT group showed a higher NRM over the no-HCT group (38.0% vs 8.7%; HR 2.08; p≤0.001), while relapse risk was lower in the HCT group (10.4% vs 29.3%; p≤0.001). In the MFC-MRDpos subgroup, relapse incidence was strikingly different in favor of HCT (9.5% vs 50.0%; HR, p≤0.001).
Conclusion: These findings suggest that in AML patients HCT could abrogate the relapse risk in patients who are MFC-MRDpos at the time of remission assessment, while the benefit from HCT was minimal in the subgroup that are MFC-MRDneg. Further study is strongly warranted to reach a clearer conclusion with a larger number of cohorts.
Lipton:Bristol-Myers Squibb: Honoraria; Takeda: Consultancy, Honoraria, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Ariad: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal